NECK-re-tie-zing FASH-e-i-tis... Say what?!
What is it? Could YOU get it? How do you spot it? Does it kill?
I originally wrote this post in September last year when I was messing around with Substack and not sure whether it was the right platform for me and my writing. I read it again a few weeks ago and I couldn’t hear my own voice in the words that I’d used. So I’ve re-written it to the extent that it’s pretty much unrecognizable from the original.
I have decided to re-issue it as a new post as I believe the content is so important. Firstly it explains what I mean when I keep referring to having been ‘sick’. But more importantly my mission these days is to spread the word about what happened to me. I hope by doing that I can educate more people to spot the early warning signs of these horrific infections and get medical help before it’s too late.
For the one person who may have read the updated original post in the past couple of weeks then apologies for the duplication.
-------------------------------------------------------------
Most of us have a hard time even pronouncing necrotizing fasciitis (NF) - the ‘proper’ name for the more sensationalist, headline grabbing ‘flesh-eating bacteria’. Its name in fact describes exactly what it is… Necrotizing means the death of tissues. And I’m talking the humankind - not the version in a Kleenex box. Fasciitis means inflammation of fascia, the tissue under your skin that surrounds your muscles, nerves, fat (like it or not we all have some), and blood vessels.
NF is categorized as a ‘rare’ disease which might lead you to think that it isn’t found very often and doesn’t kill many people. But in fact, it’s estimated that globally 150,000 people die because of NF every year. In addition, it leaves hundreds of thousands with life-changing consequences, both physical and mental. And now take this onboard - those numbers are almost certainly significantly underestimated as they’re confounded by issues with accurate diagnosis and reporting limitations.
Here in Denmark, like other Western countries, there are about 2 cases per 100,000 people per year. In our little country that’s somewhere between 100 and 150 cases a year. But that’s just a rough average as every now and again - most recently right around the time I was diagnosed - the number of cases spiked massively for a few months. That resulted in many more NF patients and far more people dying.
Research suggests that NF will kill 20% of patients in the first few days and up to 30% within a year of the infection. The number of cases is many times higher in countries with less advanced and less widely available healthcare. In those countries up to 50% of NF patients will die.
So, what causes these infections? The simple answer is bacteria. These tiny blighters are classified into different families. In the case of NF the bacteria come most commonly from the Group A Streptococcus family – in my case it was a particular type called Strep. pyogenes. These bacteria are often carried around on our bodies (skin, nose, throat) without any symptoms. Sometimes they’ll give you a minor, annoying problem like ‘strep throat’. But other times they explode and turn deadly - nobody is quite sure why.
These bacteria don’t always party alone. Some patients, including me, have other types of bacteria that have also decided to get in on the act and contribute to the infection. Then the NF is called poly-microbial.
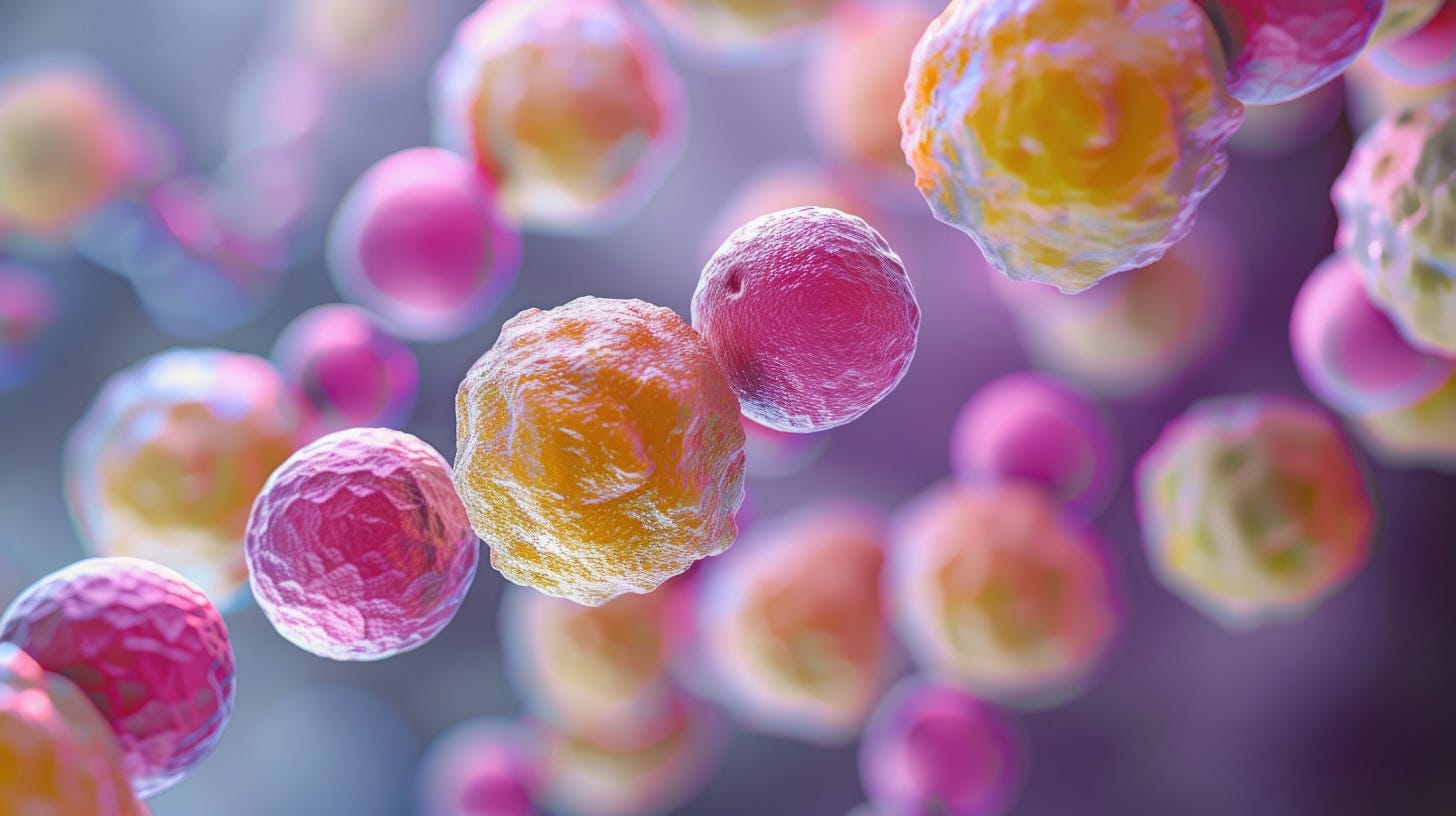
Image caption: a representation of what the S. pyogenes bacteria may look like. (Credit - Adobe Stock) Named from Greek words meaning ‘a chain’ (streptos) of berries (coccus) and pus (pyo)-forming (genes), as in some infections it causes produce pus. Under the right microscope it literally looks like a little chain of berries stuck together.
To start the process the bacteria need to get under your skin somehow. Usually, they enter the body via some kind of break in the skin. Perhaps a cut from broken glass or from shaving. A grazed knee from a fall. A scrape on your elbow when you came off your bike. An insect bite. A puncture wound from something as common as a rose bush thorn. Or perhaps an injection site. And in some instances, it gets in via a recent surgical wound.
But there’s not always an obvious break in the skin. There’s no visible route it could have taken to get into your body. Yet it did. That was me. How it got into my body remains a mystery which is unlikely to ever be solved.
Many people who get NF have other health issues. As many as 75% have one or more other health problems that lower their ability to fight an infection. They frequently have problems with their circulation, their heart, and/or their lungs. Almost half have diabetes, and nearly a third some kind of cancer.
But you guessed it, I was different once again. Like 25% of NF patients, I had none of those other health issues. I was fit and healthy. In theory NF shouldn’t have touched me, yet it did. And if it attacked me... it could attack you too.
Once NF starts it often moves fast. In many cases like mine - extremely fast. Quick diagnosis makes the difference between living and dying. When they tried to work out what was wrong with me the doctors scratched their heads and went in circles for hours. I didn’t have any risk factors and wasn’t seen as having a classic patient profile for NF. It couldn’t be that, as they wrote in my medical journal, or could it?
Correct diagnosis is so important, but it’s not easy. NF doesn’t have distinctive symptoms and easy to spot like some other diseases. It hides in the crowd with symptoms are non-specific, commonly associated with other diseases. To add to the confusion symptoms vary widely between patients.
Search the internet and you’ll read that early symptoms of NF can include things like a red and/or swollen area of skin that grows quickly - severe pain, including pain beyond that area of red skin – and maybe fever. Later symptoms could give other clues to what’s going on – skin ulcers, blisters, or black spots - pus or oozing – dizziness - fatigue – diarrhea or nausea.
Sounds OK, right? Not so hard to spot? But unfortunately, it’s not as straightforward as that symptom list might suggest.
Every NF patient story is unique. No two journeys are the same. The symptoms may show up at different times. Some never appear before you get close to dying. And sometimes the combination of symptoms will lead doctors down a rabbit hole and convince them that they’re dealing with something very different, and much less life threatening, like a common gastrointestinal bug. Too many patients have died because of incorrect assumptions. Hours, and often minutes, matter.
My first symptom was vomiting. Uncontrollable vomiting like you may have had when you were a little kid. Sudden. No warning. Repeatedly. I couldn’t even keep water down.
Then I noticed an unexplained pain in my groin - right where you’d expect a hernia. That crease between your torso and thigh. As each hour passed it got worse and worse.
That night, just 18 hours since it all started, diarrhea had joined my collection of symptoms, and the pain had become intolerable. Multiple doses of morphine failed to even make a dent in it. I was showing signs of sepsis.
Within a few hours my blood pressure was dangerously low, and I was going into septic shock.
It took just 24 hours to go from feeling fine to the brink of dying. See what I mean - it moves bloody fast.
Diagnosing NF early and acting quickly is critical when it comes to your chances of survival. Misdiagnosis is common. Many doctors will never see a case in their entire career so it’s not the first disease they would consider. My medical journal lays out the doctors’ investigative process as they tried to work out what was wrong with me. They suspected a deep vein thrombosis (a blood clot), then diverticulitis (a problem with the gut), then kidney stones, back to diverticulitis, and then a fallopian tube infection.
Only after my leg started to swell and go red (yep that was definitely not an ‘early’ symptom), and my blood infection markers skyrocketed, did NF get mentioned. Over and over again the doctors tried to talk themselves out of it. I had no risk factors. It couldn’t or shouldn’t be that.
I was fit and healthy before it all started. Even as they were wheeling me down for my first operation, they were still telling me they didn’t think it was the ‘nasty’ version. But they had to open me up to be sure. They were so wrong. And at that stage I didn’t even really understand what they were referring to when they said the ‘nasty’ version.
There’s no definitive rule book on treatment. Repeated surgeries to remove the dead, infected tissue. Liters of i.v. antibiotics pumped into your veins. And in some places, like Denmark, multiple treatments in a specialist hyperbaric chamber with pure oxygen. Did you know that oxygen is an incredibly powerful drug in its own right? More on that another time.
Research data suggests the number of cases of these infections are trending up. And I’m not talking about spikes that I mentioned earlier - I’m talking about a long-term upward trend.
Rare doesn’t mean it will never affect you or someone you love. REMEMBER the possible symptoms. REMEMBER unexplained excruciating pain. DON’T HESITATE to get medical help. Your life, or that of someone you love, might just depend on it.
If you enjoyed this post (or perhaps I should say ‘appreciate’ considering the topic) please do click on the heart, add a comment, and/or share it on as that will help more people find Hold My Hand and my writing.
COMING ON 1st MAY – my ‘book in parts’. In weekly posts I’ll be sharing my book Hold My Hand: A Journey Back to Life chapter by chapter. I’m so excited to finally share my story with a wider audience and to have the opportunity to get your thoughts and feedback.




Terrifying, Jacqui. Thanks for the low-down. I only know one person personally who had it and fortunately it was caught in time, but as you say, it can so easily be missed.